Incontinence isn’t a topic that is widely discussed, but millions of men and women suffer with it daily. Living with incontinence, which is the involuntary loss of urine or stool, can affect lifestyle and lead to feelings of embarrassment and hopelessness. Most of the time, medication, pads, and surgery are the only solutions offered to these sufferers.
We recently talked with Consortia Health cofounder Gail Page and Mary Lake Polan, MD, PhD, a professor of obstetrics, gynecology, and reproductive sciences at Yale School of Medicine, to get their expertise on incontinence, as well as alternatives to drugs and surgery.
EL | How many patients do you see per year who suffer from incontinence? What percentage of women in the United States deal with incontinence?
GP | Reports state that between 30 and 50 percent of women in general suffer incontinence when they laugh, cough, or sneeze. Urinary incontinence is a common condition in women. Approximately 25 percent of young women, 44 to 57 percent of middle-age and postmenopausal women, and 75 percent of older women experience some involuntary urine loss. Approximately 10 million men suffer from both urinary and fecal incontinence, and this is mostly due to prostate surgery or associated prostate issues.
EL | What are the main reasons incontinence develops?
MLP | Childbirth is a major reason, but also coughing and putting pressure and strain on the bladder for any reason — like jogging, horseback riding, etc.
GP | Diabetes, childbirth, obesity, excessive pressure, like Dr. Polan mentions above. There is also persistent urinary incontinence, a condition caused by underlying physical problems or medical issues, including stroke, diabetes, and Parkinson’s disease.
EL | Can incontinence be healed? How?
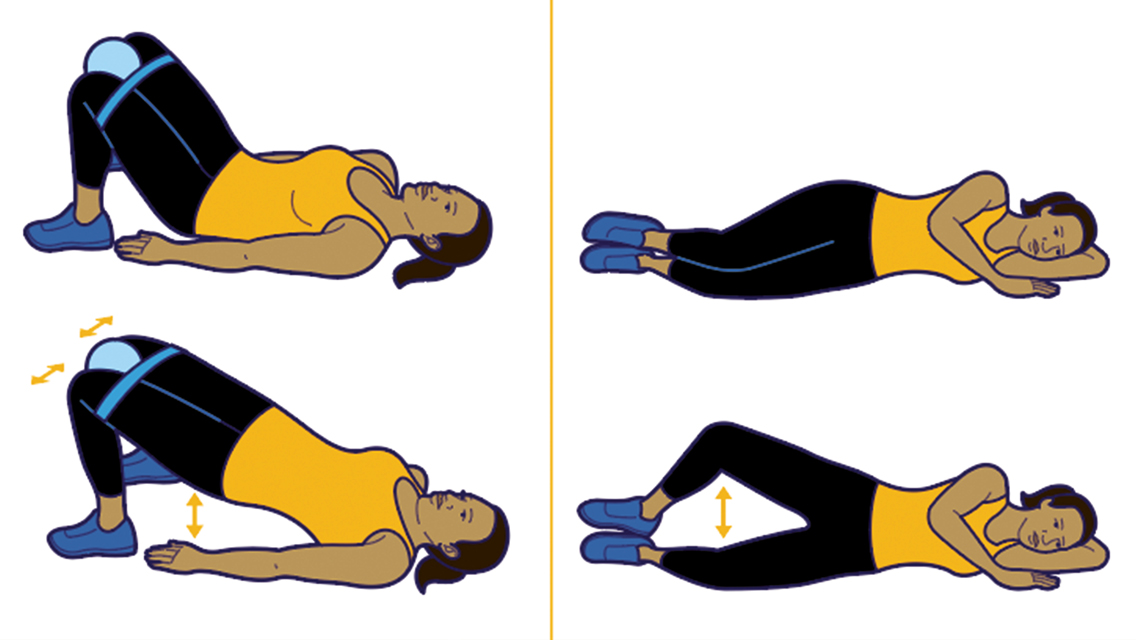
MLP | Not healed, but improved, with better pelvic-floor muscle strength by exercising the muscles — just like any other muscle in the body.
EL | How are incontinence and the pelvic floor related?
GP | Both the urethra and the rectum pass through the pelvic-floor muscles in men and women. Studies show that strengthening these muscles can greatly reduce or eliminate symptoms.
EL | What is pelvic-floor rehab?
MLP | Training the pelvic-floor muscles with feedback that teaches the woman to use the muscles to strengthen them.
GP | We use electrical stimulation in concert with electromyography to reeducate the muscles and build strength within the pelvic floor. Diagnosis, therapy, and education are key to pelvic wellness and the prevention of organ prolapse.
EL | What can women do before childbirth to prevent incontinence and pelvic-floor dysfunction? What about after childbirth?
MLP | Do Kegel exercises and learn to clench the peri-vaginal muscles. And therapy, like our process, retrains overstretched pelvic-floor tissue after a birth.
GP | Restoring a woman to pelvic health is critical, and proper education is a must. Many women do not know how to properly do a Kegel, and compliance is very difficult to attain. This is why we launched the ProPelvic solution to aid those women who have lost sensation and cannot do Kegels on their own or do not know how. This is a medical- and clinical-based innovative therapy which aids women and men in restoring strength to the pelvic floor.
EL | What is the difference in how women in the United States rehab after childbirth versus women in France?
GP | The French have a protocol very similar to the Consortia ProPelvic solution. They take a very proactive approach immediately postpartum. It is our goal to work with the healthcare system and continue to educate women about the value associated with addressing this problem proactively.
EL | And you’ve noted that men also suffer from incontinence.
MLP | Yes, they do. Sometimes after prostate surgery or from a different type of incontinence — not stress incontinence but what’s called urge incontinence, for which there are drugs.
GP | Stress incontinence is when you lose urine because of a cough or sneeze and you increase intra-abdominal pressure and it pushes the urine out. Urge incontinence is a neurological urge to void which comes out of the blue and causes you to lose urine without increasing intra-abdominal pressure. And it is treated with drugs that inhibit nerves and therefore the urge to release urine.
EL | How do men’s pelvic floors compare with women’s?
GP | The pelvic-floor muscles for both are positioned at the base of the pelvis. These muscles are internal and cannot be seen from the outside of the body in men and women. In both, these muscles are designed like a trampoline that slings across the area where you sit. They run from the pubic bone to the lower part of the tailbone and from side to side. Given our anatomy, there are differences. In women, the bones of the pelvis are wider than those of men and the bones where we sit are further apart to allow for childbirth. In general, men have a narrow pelvis and hips.
EL | What are the various long-term health effects of incontinence and pelvic-floor dysfunction?
MLP | The biggest problem is social isolation and emotional distress from fear of embarrassment.
GP | In addition, women report that they experience a lack of sexual desire, marital problems, depression, urinary-tract infections, and lack of exercise without treatment. Women often develop organ prolapse if the problem is not diagnosed and treated. It is also a leading cause of institutionalization of the elderly.
EL | Anything else you want people to know about incontinence and pelvic-floor health?
MLP | You’re in control, and there is an alternative to medication and surgery. Wearing pads can cause irritation and odor, so fixing the problem is best. Make an appointment to assess your condition — differentiate between stress incontinence and urge incontinence, so you can get the proper treatment. If you can, get ahead of the problem and reeducate your pelvic floor.
Mary Lake Polan, MD, is a clinical professor of obstetrics, gynecology, and reproductive sciences at Yale School of Medicine and chair of the Consortia Clinical/Medical Advisory Board.
Gail Page is the cofounder of Consortia Health, a personalized medicine company providing an integral delivery model in partnership with physicians to provide diagnosis, treatment, and educational support to address pelvic-floor disorders.


This Post Has 0 Comments