When most people think about the pelvic floor, if they do at all, they often just consider its starring role in childbirth. But this hammock-shaped collection of muscle and connective tissue is key to our everyday functioning: It supports the internal organs of the pelvis and abdomen, helps control the bladder and bowels, and allows for healthy sexual function in everyone, regardless of age or gender.
“The pelvic floor is the Grand Central Station of the body,” says pelvic-floor physical therapist Riva Preil, PT, DPT, author of The Inside Story: The Woman’s Guide to Lifelong Pelvic Health. “When the pelvic-floor muscles are at a happy resting tone — when they’re not overstretched and weak, or in spasm and tight — they can perform those functions for you.”
For many people, however, the pelvic floor does not work the way it’s supposed to. According to the Mayo Clinic, about 32 percent of women and up to 16 percent of men experience at least one pelvic-floor disorder in their lifetime. And while there is a dearth of related statistics on transgender and gender-diverse communities, gender-affirming practices and surgeries can have an impact on the pelvic-floor muscles.
“The pelvic floor is the Grand Central Station of the body.”
Common symptoms of pelvic-floor dysfunction include pelvic pain, urine leakage, constipation, and lower-back pain, Preil explains. The Cleveland Clinic notes that women and those assigned female at birth may feel pain during sex, and men and those assigned male at birth may struggle to get or keep an erection.
If you’re experiencing these or other problems related to the pelvic floor, rest assured that there are strategies to relieve pain, weakness, and tightness, and to restore normal muscle function. And even if you’re free of these symptoms, these strategies can help you prevent future issues from cropping up. What follows are experts’ top tips for taking care of these often-overlooked muscles.
Anatomy of the Pelvic Floor
The pelvic floor is where your abdominals and legs converge, and where ground-reaction forces are absorbed with each step you take, says Preil. It’s a group of muscles that form a sort of hammock or sling. Sitting at the bottom of the core (which includes the abdominal, back, and diaphragm muscles), these muscles are supported by bones, connective tissue, and fascia.
Muscles of the Pelvic Floor
The levator ani forms the bulk of your pelvic-floor muscles. It’s a funnel-shaped structure that supports bowel, bladder, and sexual function and keeps your pelvic organs in place. It wraps around the entirety of your pelvis, and it forms from the confluence of three separate muscle components:
- The pubococcygeus runs from the pubic bone to the center of the perineum. It controls the flow of urine, aids in ejaculation, and helps position the fetus’s head during childbirth.
- The puborectalis forms a sling around the rectum and assists with defecation.
- The iliococcygeus is a thin sheet of muscle that spans the pelvic canal and connects to the sacrum and coccyx. It provides a secure anchor point for the pelvic floor.
- The coccygeus is a smaller, triangular-shaped muscle located toward the back of your pelvis that helps support the pelvic organs and, with the levator ani, comprises the pelvic diaphragm.
(Anatomically correct diagrams of male and female pelvic floor muscles are available through the Mayo Clinic.)
Bones of the Pelvis
- The coccyx, also known as your tailbone, is a small triangular bone at the base of your spine. It serves as an attachment site for pelvic-floor muscles.
- The sacrum is located just above the coccyx. This shield-shaped bone acts as a muscle attachment site and helps stabilize the pelvis.
- The hipbones are located on either side of your pelvis and serve as another attachment site for pelvic-floor muscles. Each hipbone consists of three separate bones: the ilium, ischium, and pubic bone.
The 5 S’s of Pelvic-Floor Function
The “Five S’s” is a mnemonic encompassing the five major functions of the pelvic floor.
- Support: The sling of muscles, fascia, and ligaments supports the organs inside the abdominal cavity and the pelvis, which include the sexual organs, bladder, and intestines.
- Sphincter: The pelvic-floor muscles allow for the appropriate opening and closing of the urethral and anal sphincters, ensuring successful urination and bowel movements while simultaneously preventing leakage of urine and fecal matter.
- Sex: The pelvic floor muscles relax and contract, allowing for penetration, arousal, and orgasm.
- Stability: The pelvic floor stabilizes the torso and allows for dynamic movement of the extremities. It plays a central role in breathing and regulating pressure in the intra-abdominal cavity.
- Sump pump: The pelvic floor helps move blood and lymph fluid through the pelvis and up into the trunk of the body.
Causes of Pelvic-Floor Dysfunction
Lifestyle, age, and major life events like surgery and childbirth can affect pelvic-floor function. These are a few of the factors to consider as you strive to keep these muscles working properly.
- Stress. “People inadvertently hold tension and tightness in their pelvic-floor muscles,” Preil says. It’s like how you might clench your jaw or let your shoulders creep up toward your ears. In fact, there is a strong connection between pelvic-floor dysfunction and temporomandibular joint dysfunction (TMJ). If you notice you’re clenching your jaw, you may also be clenching your pelvic-floor muscles, she notes.
- Age. Muscles tend to weaken and become harder to strengthen as we get older, a concept known as sarcopenia. The pelvic-floor muscles are no exception, says Megan Rorabeck, DPT, a board-certified women’s health clinical specialist and author of Between the Hips: A Practical Guide for Women.
- Pregnancy and childbirth. The pelvic-floor muscles and tissues can become strained and weakened during pregnancy and vaginal delivery.
- Hormonal changes. The reduced production of estrogen during menopause can contribute to the pelvic-floor muscles becoming weaker and frailer, says Rorabeck. “Any issue we might have had in our younger years that we could skate by can become a big deal with that hormone change.”
Anyone undergoing gender-affirming hormone therapy could see tissue changes, such as testosterone-induced vaginal atrophy, that are like postmenopausal changes in cisgender women, according to Brigham and Women’s Hospital. Those changes can impact bladder, bowel, and sexual function. - Muscle strain. Bearing down when going to the bathroom or excessive coughing can strain your pelvic-floor muscles, causing weakness.
- Issues in other areas of the body. The pelvic-floor muscles connect with the spine and hips, and any weakness, tightness, or dysfunction in these areas can affect the pelvic region. “If somebody has low-back or hip pain that isn’t getting better with a traditional orthopedic approach, it could be that the pelvic floor is getting missed,” Rorabeck explains.
- Trauma. Sexual abuse or assault, car accidents, and other physical injuries can result in pelvic pain and dysfunction.
- Surgery. Surgery in the pelvic region, such as a cesarean section (C-section), gender-affirming procedure, hip replacement, or prostatectomy (removal of the prostate), can cause scarring that might attach to skin, muscle, or connective tissue, restricting blood flow and leading to pain. Such surgeries can also cause the pelvic-floor muscles to weaken.
- Gender expression and affirmation. Techniques that have a significant beneficial effect on quality of life and mental and emotional health, such as tucking and binding, can often also cause pelvic-floor pain or dysfunction.
- Bicycling. Sitting on a bike seat puts a lot of pressure on the pelvic floor. As a result, “cyclists tend to develop tight pelvic-floor muscles due to the biomechanics of cycling,” notes Brooke Cates, founder and CEO of The Bloom Method, a pre- and postnatal fitness program.
Symptoms of Pelvic-Floor Dysfunction
With so many factors affecting a naturally complex region of the body, it’s little surprise that pelvic-floor dysfunction doesn’t look the same for everybody. In fact, Preil says, there are two broad categories of dysfunction: At one end of the spectrum is pelvic-floor tightness, or overactivity; at the other end is pelvic-floor weakness, or underactivity.
Pelvic-Floor Tightness:
A common symptom of tightness is often feeling like you need to pee. This happens because the muscles around the urethra (the tube that empties urine from the bladder) are tense and overactive. “The muscles never fully relax when you’re trying to urinate, so you constantly feel like there’s still more urine in the bladder,” she explains.
Or, you may be constipated — another symptom of overactivity — except it’s the muscles around your rectum (the last several inches of the large intestine) that are tight.
Some people with pelvic-floor tightness may also notice that they can’t stay erect during sex, says Preil. “Male sexual functioning is so dependent on blood flow, and if muscles are tight, it can restrict that blood flow.”
Pelvic-Floor Weakness:
On the other end of the spectrum, a telltale sign of pelvic-floor weakness is urinary incontinence, or difficulty holding in your pee. “That’s when you have those experiences of running or jumping on a trampoline with your kiddo, and you pee yourself a little bit,” says Cates.
Another symptom of weakness is pelvic-organ prolapse, which occurs when one or more pelvic organs (the uterus, bladder, or rectum) drop into the vagina or bulge into the anus, causing discomfort. “Women will report a feeling of fullness in the pelvic floor, almost like a tampon is only partially inserted,” Preil explains.
Cates notes that either category of pelvic-floor dysfunction could lead to the same symptoms; leaking urine, for instance, could be caused by tightness or weakness.
Moreover, Preil adds, people can experience both tightness and weakness at once. And it’s possible that one could lead to the other (i.e., if left unchecked, tight and overactive muscles can become weak).
3 Strategies for Improving Pelvic-Floor Health
There are myriad factors that can compromise the health of your pelvic floor, but there are just as many approaches you can take to lower the probability of experiencing issues. Use the following three strategies to keep these muscles healthy and functional for life.
1. Retrain your breathing.
A simple way to improve pelvic-floor mobility and function is to shift to diaphragmatic breathing. During a natural breath, “when you take a deep inhale, the respiratory diaphragm and pelvic-floor diaphragm both descend,” says Meagan Corrao, PT, DPT, a certified pelvic-rehabilitation practitioner and clinical specialist with Northwell Health Rehabilitation Network. On the exhale, they both rebound to their usual position.
To breathe diaphragmatically, focus on expanding your abdomen on the inhale, aiming to fill your ribcage and back. “Imagine if you were to blow air into a balloon, all parts of the balloon expand,” Rorabeck says. “When you breathe into your belly, think of the belly and the pelvic floor expanding together, like the balloon.” (Get step-by-step instructions below in “6 Exercises for a Healthy Pelvic Floor.”)
She recommends first practicing diaphragmatic breathing while lying in bed at night to get the hang of it. That way, you can more easily tap into this approach when you’re stressed and anxious or you notice you’re clenching your jaw. “To be effective at doing it in the heat of the moment when our body needs it most, we have to be able to fall back on some muscle memory.”
2. Exercise to strengthen and lengthen.
Performing exercises that stretch and strengthen your pelvic-floor muscles can help you prevent overactivity and underactivity.
Kegels are perhaps the best-known pelvic-floor exercises: You squeeze, hold, and relax your pelvic-floor muscles.
Kegels can be an effective exercise for strengthening the pelvic floor, but they’re often done incorrectly. “For some reason, when we train the pelvic floor, we only think Engage, engage, engage; contract, contract, contract,” Cates says. Constantly contracting the muscles without also relaxing them can create or worsen muscle tightness.
Kegels can be an effective exercise for strengthening the pelvic floor, but they’re often done incorrectly.
If you’re going to do Kegels, it’s important to train both phases of the movement: Contract the pelvic-floor muscles, then relax them fully. “Get to a point where you can do that in a fluid motion, just like you would in a biceps curl,” she suggests.
Learning how to engage and relax these muscles isn’t intuitive for everyone. Give yourself time to practice building awareness and control, and don’t hesitate to seek professional help for additional guidance. (For more stretching and strengthening exercises, see “6 Exercises for a Healthy Pelvic Floor” and “Pelvic-Floor Devices for Training Muscles” below.)
3. Seek professional support.
There are many types of healthcare providers you can consult — including obstetricians and gynecologists, urologists, physical therapists, pelvic-floor specialists, and gastroenterologists — for pelvic-floor issues.
Common indicators that something’s not quite right in the pelvic-floor region are pain during sex, urinary or fecal incontinence, a feeling of heaviness in your pelvis, frequent urination, difficulty staying erect, constipation, or lower-back pain.
If it turns out you have pelvic-floor dysfunction, you’ll likely work with a pelvic-floor physical therapist to rehabilitate. The initial consultation may include a pelvic exam during which the therapist inserts a finger vaginally or rectally to check muscle tone, strength, and endurance, Corrao says. They may also analyze your posture, walking mechanics, breathing patterns, and flexibility and strength in your core, arms, and legs.
The more we normalize pelvic health, the less stigma and shame we attach to it.
Using this information, the therapist develops a treatment plan. “Most patients start with a home exercise program from day one,” she notes. Some may need flexibility, relaxation, and breathing exercises, while others need strengthening, core, and posture exercises.
Many people don’t like asking for help with pelvic issues. Some are embarrassed to admit they leak pee or can’t maintain an erection. Others haven’t felt heard by healthcare providers when they bring up their pelvic issues at medical appointments.
Thankfully, the field of pelvic health is expanding. “Each year, more providers are going into this field, and it’s becoming more well-known and talked about,” Preil says. The more we normalize pelvic health, the less stigma and shame we attach to it.
6 Exercises for a Healthy Pelvic Floor
Your pelvic-floor muscles are like any other muscles in your body: They benefit from being strengthened and stretched often through regular movement and function.
But it’s not enough to focus only on the pelvic-floor muscles — you also must train the abdominal and diaphragmatic muscles surrounding the pelvic floor. “They all relate to one another in terms of how they function,” says Alyssa George, PT, DPT, a physical therapist with Motion Minnesota who specializes in treating pelvic and orthopedic conditions.
Performing a combination of stretching and strengthening exercises can keep your pelvic floor strong and mobile. The following routine was codesigned by George and her Motion Minnesota colleague Britta Gauthier, PT, DPT, who specializes in pelvic-health and orthopedic rehabilitation. Incorporate the mobility exercises into your routine daily and the strength exercises up to three times per week.
If you experience pelvic pain or you’re already being treated for pelvic-floor dysfunction, consult a healthcare provider before performing these exercises.
Breathing and Mobility
Include these exercises in your daily routine.
Diaphragmatic Breathing
This form of breathing taps into your pelvic-floor muscles and prepares them for the moves that follow.
Perform one set of 10 breaths.
Full Instructions
- Lie on your back with legs bent or extended. Place one hand on your stomach.
- Breathe in deeply, feeling your belly push against your hand as it expands.
- Exhale fully, allowing your belly to draw in.
Pelvic Floor Contract and Release
Kegel exercises are effective for strengthening and lengthening the pelvic floor.

Perform one set of 10 breaths.
Full Instructions
- Lie on your back with your knees bent and feet on the floor, arms resting at your sides.
- Aim for a neutral pelvis position (not tucking your tailbone or excessively arching your back).
- Squeeze and lift your pelvic-floor muscles; imagine there is a string drawing your perineum up and in.
- Hold briefly and then release your pelvic-floor muscles with control.
- Allow the muscles to relax fully before repeating the contraction.
Cat–Cow
This classic yoga move increases lumbar (lower-spine) mobility, which is critical for pelvic-floor function.
Perform one set of 10 reps.
Full Instructions
- Begin on all fours with your shoulders stacked over your wrists and knees bent 90 degrees.
- On an inhale, slowly curve your lower back and tilt your pelvis up, allowing your belly to drop toward the floor.
- As you exhale, draw your belly in and gently arch your back up toward the ceiling.
Strength
Body-Weight Squat
The glutes and the pelvic floor are buddies, George says. A body-weight squat strengthens the glutes; learning to coordinate the movement with breath can help lengthen the pelvic floor.
Perform two sets of 10 reps.
Full Instructions
- Stand with your feet slightly wider than shoulder width apart.
- Inhale diaphragmatically. As you do, bend at your knees and hips and squat down until your knees are close to a 90-degree angle.
- Keep an elongated spine; don’t let your knees creep over your toes. On an exhale, stand back up by straightening your knees and hips simultaneously. Repeat.
- To progress the move, hold a dumbbell in each hand, with your arms extended at your sides.
Dumbbell Deadlift
Coordinating your breath with this classic hip-hinge exercise teaches you how to pick up heavy objects without holding your breath (holding your breath during a heavy lift is a common precursor to urine leakage).
Perform two sets of 10 reps.
Full Instructions
- Stand with your feet shoulder width apart, holding a medium-heavy dumbbell in each hand in front of your thighs. Choose a weight that is challenging for you and that you can use to perform all 10 reps with great form.
- Inhale diaphragmatically. As you do, bend your knees slightly and hinge at the hips to lower the dumbbells toward the ground. Keep the dumbbells close to your legs.
- On an exhale, stand back up by straightening your hips and knees simultaneously.
- Fluidly flow from one position to the next, trying not to hold your breath at any point. Keep your abdominal muscles engaged and your back straight during the exercise.
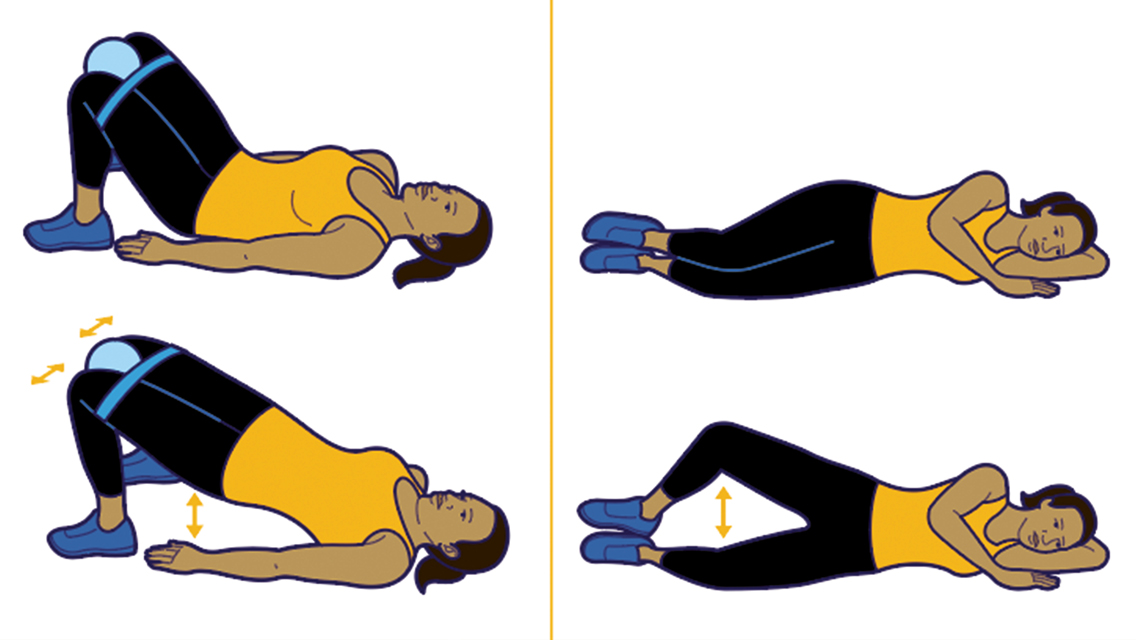
Banded Side Steps
This exercise targets the side-butt muscles that play a key role in pelvic-floor function.
Perform five sets of 10 reps in each direction.
Full Instructions
- Stand with a small, closed-loop resistance band around either your lower legs (just above the ankles) or around your thighs (just above the knees).
- Bend your knees slightly so you’re in a quarter-squat position.
- Slowly step sideways, maintaining tension in the band.
- Continue stepping in one direction until you’ve completed 10 reps. If you’re tight on space, alternate sides with each rep.
Pelvic-Floor Devices for Training Muscles
In addition to standard stretching and strengthening exercises, there are devices that can help you train your pelvic floor. Megan Rorabeck, DPT, recommends two tools for relaxing overactive pelvic-floor muscles: a dilator set and a pelvic-floor wand.
Dilators are tube-shaped devices that come in kits with dilators ranging from small (about the size of a finger) to large, according to the Memorial Sloan Kettering Cancer Center. These can be inserted vaginally or rectally and left in place for 10 to 15 minutes to stretch the muscles. Wands are similar in that they’re inserted vaginally or rectally, but they’re curved to target the deeper muscles in the pelvic floor.
You can find and buy these devices online, but Rorabeck recommends first consulting a pelvic-floor physical therapist to ensure you’re getting a device that fits your needs. Plus, the therapist can show you how to use the device most beneficially.
In addition to devices like wands and dilators, there are vaginal weights for pelvic floor strengthening; these tools are inserted vaginally and held in place by the muscles. However, Rorabeck does not usually recommend these. “People often unintentionally cheat,” she explains. “They tilt their pelvis, clench on with their butt muscles, press their thighs together, or walk rigidly to hold the weight in place.”
Instead, she prefers that her patients perform functional movements with dumbbells, kettlebells, or plyometrics (jumping exercises). (For a primer on functional movements and training, see “Ready-for-Anything Fitness.“)





This Post Has One Comment
How about making a version of this for men, please?