How do you measure your health?
Our annual physicals are indeed essential, as they offer us a basic check-in on certain numbers. However, because there’s so much more to the story than what standard tests gauge, I encourage my clients to also regularly look deeper with additional assessments.
When we’re interested in getting a sense of where we’re at health-wise and what kind of progress we’re making (or not making), there are certain numbers that simply tell us more than others. In some cases, that means more detail around the basics. In other cases, it means examining added dimensions that conventional screening doesn’t cover.
Many of these extra assessments don’t cost anything. In fact, there’s one you can even do before you finish reading this article. Check out the 10 I typically suggest for my clients to gain a clearer picture of their current health status.
1. Lifestyle
As simple as this one seems, your answers to these five questions tell you (and me) quite a bit about the path your health may be on. Ask yourself:
In the past seven days, how many days have you . . .
- Gotten at least seven hours of uninterrupted sleep?
- Eaten at least five cups of fresh produce, at least three cups of which were non-starchy vegetables?
- Consumed at least two liters of water?
- Been physically active for 30 minutes?
- Practiced at least five minutes of conscious relaxation, meditation, or gratitude?
These are five straightforward, telling questions that help give you an overall picture of your daily patterns. If your answer was less than four days for any of them, then that’s an indicator of which lifestyle areas could use your added effort. No further testing is needed to get started.
2. One-Mile Run Time or VO2Peak
Remember the Presidential Physical Fitness program in grade school? I hated the sit-and-reach, but loved the one-mile run. I was a top-tier performer back then and I intend to keep it that way because this simple run turns out to be a great predictor of overall mortality risk.
Peak exercise capacity (expressed as METs by most studies) is a better forecast for death risk than overall fitness — even if one has other concerns such as a body mass index greater than 30, diabetes, elevated blood pressure, or high cholesterol. Within each of those groups, the individuals who could crank out eight METs for 8 to 12 minutes had about half the relative risk of dying compared to those producing less than five METs.
If you don’t know your METs, you can figure it out pretty easily if you know your VO2peak. Simply divide your VO2peak by 3.5. Judging by my latest Active Metabolic Assessment in which my peak oxygen consumption topped out at 52 ml/kg/min, or nearly 15 METs, I still got it!
If you don’t know your METs or VO2 peak, check if you are fit enough to qualify for active military duty (another standardized fitness test) by running/jogging two miles in under 18 minutes.
3. Resting Heart Rate and Heart-Rate Variability
Let’s say you passed the lifestyle questionnaire with flying colors and you’re already physically fit by the standards of peak exercise capacity. You may still want to understand why you aren’t losing fat or gaining strength in accordance with what you’d expect.
In some cases, it could be that you’re pushing your body too far past its red line: The total amount of stress accumulating in your body and mind may be standing in the way of positive adaptation.
We can only push our bodies to adapt in a positive way if we’ve recovered from the last bout of stress. Resting heart rate (RHR) and heart-rate variability (HRV) are arguably the best ways to gauge the body’s day-to-day readiness for more stress. Lower RHR and higher HRV (which indicates better recovery or readiness) are significantly correlated with longevity.
Sure, you can pick your workout based on whether or not your muscles are sore, but your nervous system — which ultimately controls RHR and HRV — has the final say in how your body responds to that workout. Pile too much physical stress on top of other life obligations and you could be in the hurt tank for a few days.
4. Body Composition
During every doctor visit, they probably measure your height and weight and chart your body mass index (BMI). Unfortunately, BMI means very little over time because it isn’t sensitive enough to express the relationship between lean body mass and fat mass. Medical treatment guidelines operate using BMI data, but there is plenty of good evidence supporting more sensitive body composition markers as indicators for optimal health.
The entire health conversation in this country is sadly focused on being lighter rather than leaner. Instead of getting our doctors’ encouragement to lose fat and gain muscle, we are solely told to lose weight. And rather than celebrating strength gains, we get discouraged when the scale remains stagnant.
When you speak to a Life Time fitness professional, you’ll notice they may give very little thought to your weight or BMI, but care a whole lot about your body composition (body fat expressed as a percentage of total weight). (If you’re interested in finding out your own body composition levels, we welcome you to schedule a consultation with one of our fitness professionals.)
We all want to aim to build and maintain substantial muscle tissue to help us reduce our risk of bone loss, falls or fractures, type 2 diabetes, and other forms of metabolic meltdown.
How do you know if you’re headed for a meltdown? You’ve got to test for them.
Unfortunately, annual check-ups oftentimes won’t uncover major concerns until it’s too late — as in, “time for medication” too late with the onset of chronic disease. Standard blood chemistries and basic health measures are meant to be disease screening steps at best, as opposed to a measure of how you compare to your peak potential.
That means there can be unaddressed symptoms and signs that indicate your metabolism is drifting away from its physiologic potential before a standard test ever picks it up: your energy has plummeted, physical recovery takes a long time, mental sharpness eludes you, and your resiliency to stress is about as strong as a wet paper bag.
What could those symptoms be caused by or lead to? That depends. To find out, I’d first suggest evaluating the next six assessments on this list.
5. Nutrient Levels
Nothing drags down your mood or immunity quite like low levels of the sunshine vitamin, AKA vitamin D. Beyond vitamin D, however, I recommend people also assess other important nutrient indicators.
Aim to test your vitamin D levels at least annually and supplement accordingly. Anyone with complaints of low energy, little activity tolerance, or trouble losing weight would also want to assess their iron levels at least every six months. Those who experience slipping mental performance or concerns over extended soreness ought to think about testing their essential fatty-acid levels to determine omega-3 dosing needs.
Beyond these basic nutrients, there may be more extreme cases in which someone may want to assess their coenzyme Q10 levels, red-blood-cell magnesium, or other nutrients, for example.
6. Fasting Insulin Levels
There may not be a better way to head off diabetes and jump-start fat loss than to understand your glucose and insulin dynamics. You can do this by testing fasting insulin levels. Ideally, the level of this hormone should settle well into single-digit levels after a night of rest.
Some proactive healthcare providers initiate aggressive nutrition and lifestyle change protocols when insulin levels drift into the double digits and for good reason — insulin resistance usually develops as a gradual process over 10 to 30 years before fasting blood-sugar levels show abnormalities.
You can ask your provider to assess your fasting insulin levels, or you can do it through direct-to-consumer lab testing in most states as well.
7. Cholesterol Particles
Cholesterol is inherently helpful to our bodies: It’s a vital repair substance for our arteries and supports our brain function. Without it, every cell in our bodies would eventually die. In the absence of inflammation, cholesterol cannot be harmful. Just as food quality is likely more important than food quantity (calories), how your body transports cholesterol appears to be more important than the total amount. Standard cholesterol profiles fail to show that level of detail, though.
Any individual who is concerned about their cholesterol-inflammation-heart disease risk would want to monitor cholesterol particle size and particle number as well as inflammation markers on a regular basis. The test of choice to find these would be a Nuclear Magnetic Resonance (NMR) plus high-sensitivity C-reactive protein (CRP-hs) and homocysteine.
This method may be more telling, as nearly half the individuals who suffer heart attacks have completely normal cholesterol using standard testing methods. Carrying cholesterol in small, dense particles (as opposed to larger, fluffy particles) makes it easier for the waxy substance to burrow into artery walls and become oxidized, ultimately triggering the immune system to attack the vascular wall to create an irritated plaque-like scar tissue.
Assuming cholesterol automatically causes heart disease is like blaming firefighters for setting fires. Where there’s a fire, there will always be firefighters, but where there are firefighters, there isn’t always fire.
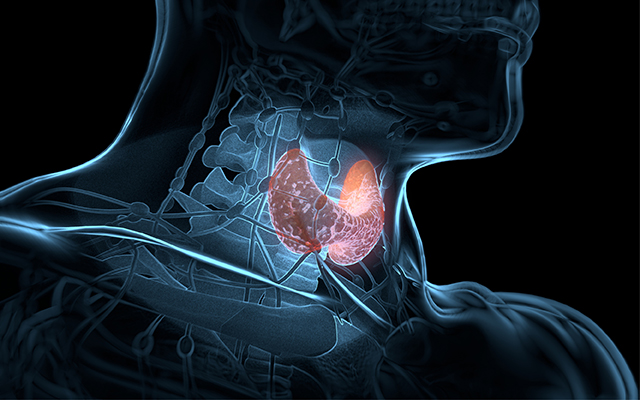
8. Thyroid Hormone Levels
Interestingly, high cholesterol levels were once used as a diagnostic measure to determine if someone had an underactive thyroid. When overall metabolism slows (a characteristic of underactive thyroid hormones), cholesterol metabolism also slows, causing cholesterol levels to noticeably rise.
When people (mostly women, unfortunately) report depression-like symptoms, cold hands and feet, hair loss, brittle fingernails, weight gain or stubborn weight loss, or constipation, they will often have their Thyroid Stimulating Hormone (TSH) screened. However, this doesn’t give a comprehensive indication of metabolic function related to all of the thyroid hormones. Too often, TSH is monitored as it slowly creeps up for a few years (while the above symptoms nag the individual in debilitating ways) until it’s high enough to warrant medication.
To head off the lengthy time period of unpleasant symptoms (just as with the insulin resistance and cholesterol-inflammation patterns mentioned), it’s usually better for patients to seek the deepest level of testing up front and request to have their free T4 and free T3 levels tested along with TSH. This way, the thyroid hormone pattern can shed light on more specific nutrition, lifestyle, and supplementation recommendations to compliment or preempt the need for medication in the future.
9. Free and Total Testosterone
While underactive thyroid may be rare in men, more often men experience their own brand of unhealthy hormonal changes. If you notice body fat accumulating in the belly and chest areas, it may be time to check in on your testosterone dynamics.
Total testosterone levels, however, don’t tell the whole story. Men looking to maintain top-tier levels of muscle mass and vitality will find it best to monitor their own trends of both total and free (active) testosterone levels over time.
“T” activity doesn’t just dictate muscularity; it also has significant impacts on mood and overall metabolic function, primarily insulin sensitivity. Low testosterone activity may be able to hint at early insulin resistance patterns, especially when trended from early or mid-twenties. Since about one-fourth of men in their late 30s have low testosterone and about one-third of American adults have insulin resistance, there’s a great deal of overlapping lifestyle and metabolic patterns these two conditions share. Test one or test both, but at least test something if you don’t feel like you.
10. Happiness
This final health measure could have fallen anywhere on this list, but I put it here to leave you with an easy-to-measure-but-hard-to-maximize metric. Beyond the physical assessments and biochemical screenings, there’s the question of emotional well-being — happiness.
Even people who aren’t setting the curve on the earlier tests I mentioned or who have sub-optimal patterns in certain physical areas can still outlive their peers if they meet everyday life with a positive mindset. If we’re truly happy, we have better psychological resilience and mental fortitude to overcome any of these other challenges.
How do you test it? There are all kinds of surveys available online to screen for depression, and entire lists of happiness questionnaires. However, the best assessment tools might be a pen, notebook, and time for self-reflection. Just as we can track our health measures and physical achievements, we can gauge our personal growth and well-being over time. Likewise, we can gather support for this dimension in our journey as we do for our physical health.
There’s genuine power in clarity — no matter what number or capacity we’re measuring. What we honestly assess is what we’ll most likely invest in. Whatever tests and tools you choose to access, don’t stop seeking the best for yourself!