Robert Hedaya tried everything in mainstream psychiatry’s toolbox to treat a patient with panic disorder, including cognitive behavioral therapy and a series of prescribed medications. She was still having attacks after a year, though, so Hedaya went back to the lab to look at her case from a different perspective.
“Early in my training in psychiatry at Georgetown, I figured out that the way things look depends on the lens you use,” says Hedaya, MD, ABPN, DFAPA, founder of the National Center for Whole Psychiatry and clinical professor of psychiatry at Georgetown University School of Medicine. “If you use a low-powered lens to look at mental illness, you look at communities and culture. If you use a medium-powered lens, you look at family systems. If you use a high-powered lens, you look at molecules.”
He revisited the patient’s blood work and saw that her red cells were larger than normal. He did a literature search and found that a deficiency in B12 could be the cause, so he began a series of B12 injections. Within days, the panic attacks were over.
Now, Hedaya practices what he calls “whole psychiatry.” New patients undergo a four-hour workup, in which Hedaya examines all the factors that have combined to cause a break in a person’s mental health. Unlike his colleagues in mainstream psychiatry, he conducts extensive lab work to look for disruptions in basic body systems that might manifest as mental illness, while also looking into psychological, social, and spiritual factors.
“These are the same [disruptions] that underlie the chronic illnesses of Western society,” he explains. “Take inflammation, for instance: In one person, it might show up as diabetes, in another person as cardiovascular disease, in someone else as depression.”
Integrative psychiatrist and author Hyla Cass, MD, concurs. “Psychiatry is the only specialty that doesn’t test the organ involved, namely the brain,” she says. “If you have heart disease or hepatitis or diabetes, doctors will perform lab tests to monitor the system in question and treat accordingly. But if your inflamed brain shows symptoms of mental illness, all of a sudden they don’t consider the brain an organ anymore — they think we have to talk people out of that illness. Talk therapy and even the psychiatric medications can be helpful, but first we have to approach the biochemical root cause.”
Hedaya and Cass are part of a growing number of mental-health professionals who find the mainstream approach to mental illness insufficient. Many psychiatrists spend less than an hour evaluating a new patient and base their diagnosis and treatment plan on the symptoms that the patient reports and that they themselves see during the exam. Sometimes they will order scans to make sure a physical disorder — like a mass in the brain — isn’t causing the symptoms, but mostly they match the symptoms to a medication and, sometimes, recommend psychotherapy.
Integrative psychiatrists, on the other hand, might use these medications to stabilize a patient who is in a crisis state. Their overall goal, however, is to treat the underlying health issues through nutrition, supplementation, and lifestyle changes.
Treating the Whole Person
Curing patients with vitamins, as Hedaya did with the woman suffering panic attacks, is not new. In fact, this approach was the breakthrough treatment in mental health in the 1950s. Canadian physician and medical researcher Abram Hoffer began treating people with schizophrenia using niacin, or vitamin B3, and claimed a cure rate of 75 percent — meaning, he said, that these people were well enough to go back to work and pay taxes instead of needing to be supported by society. In 1968, Nobel Prize–winning scientist Linus Pauling — the great champion of megadose vitamin C — coined the term “orthomolecular,” which means “the right molecule,” to describe this method of treatment.
The ’50s also saw the introduction of the prescription drug Haldol and other such medications, and they were widely embraced by the medical profession over the years. But recently, there has been growing frustration with drug therapy among doctors as well as patients — the cure rate is abysmal and the side effects so vicious that even patients who feel better don’t want to continue the regimen.
According to Steven Carter, director of the International Society for Orthomolecular Medicine, those who advocate for high-dose vitamin treatments, as opposed to drug therapy, use nutrients that occur naturally in the body. And there are 40 essential nutrients that need to be balanced according to someone’s individual biochemistry.
“Medications can be quick,” says Jonathan Prousky, ND, MSc, editor of the Journal of Orthomolecular Medicine. “They will quickly subdue someone and make them docile, which makes people think they’re getting better. But they’re not getting better. I’ve never met a patient on an antipsychotic medication who was living a thriving, flourishing life. I’ve never seen it.”
There is a relative scarcity of research into the healing properties of vitamins and nutrition, because, frankly, there’s little profit to be made from these discoveries — unlike the money flowing from new FDA-approved drugs. Even worse, there is not enough awareness of the existing research, says Jeffrey Becker, MD, a Los Angeles psychiatrist and practitioner of functional medicine who specializes in schizophrenia.
Still, Becker and others are gathering this research and crafting multilayered treatment strategies that are proving effective even with schizophrenia, one of the most intractable and complex of mental illnesses. “With schizophrenia, it’s as if the dream world is penetrating your everyday consciousness,” he says. “All of us have the capacity to ‘hear voices’ — we do it in our dreams. In this disorder, it happens when it shouldn’t.”
“All of us have the capacity to ‘hear voices’ — we do it in our dreams. In this disorder, it happens when it shouldn’t.”
Scientists believe that numerous genetic flaws create the propensity for schizophrenia, which may then be triggered by some form of stress, such as illness or extraordinary environmental pressures. In addition, people with schizophrenia and other mental illnesses often have lifestyles that compound the biochemical storm within. They frequently overuse stimulants and they smoke, which inactivates vitamin B6, depletes other nutrients, and increases oxidative stress. And they often have poor diets.
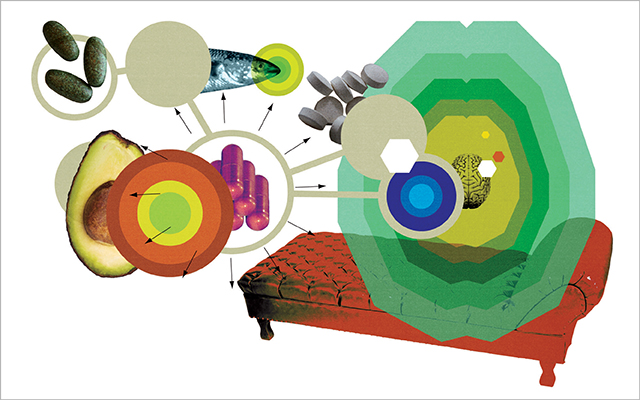
Integrative psychiatrists approach schizophrenia and other mental illness by treating the whole person, examining their problems through the different lenses that Hedaya describes. They urge them away from drugs, alcohol, and smoking; encourage exercise and a good night’s sleep; suggest healthy ways of connecting to other people, nature, and a spiritual practice; and combat biochemical imbalance with an array of supplements and other nutritional interventions (see next page for specific nutritional tips).
The good news is that when problems of the brain are treated with a whole-body approach, issues in other parts of the body often resolve. “Sometimes their skin clears up,” says naturopath Ray Pataracchia, ND. “Their energy level picks up. I had one client who said that everyone at work teased him because his abdomen looked like a basketball. When I treated him, his digestion improved and the ‘basketball’ went away.”
Not everyone seeking help for his or her own mental illness or that of a loved one can find a clinician committed to this whole-body treatment, but any committed clinician can learn the science behind these approaches. “All this is complicated, but it’s not rocket science,” says Becker. “It should be taught to psychiatrists, but it’s not. I had to learn it all on my own; most of the information is out there on PubMed.”
Patients and their families shouldn’t be shy about pushing their clinicians to look beyond the latest wonder drug and try to incorporate some orthomolecular strategies. “Patients should compel their doctors to prescribe vitamins,” says Andrew Saul. “Manage the doctor; don’t let the doctor manage you. It’s your body, your life, and the doctor works for you.”
Nutrition for Schizophrenia
What follows is a series of nutrition-based strategies integrative psychiatrists use to treat schizophrenia, one of the most perplexing of mental diagnoses.
Fatty Acids
Our brains are 60 percent fat and require a diet rich in fatty acids to maintain the integrity of cell walls. “Fats embed themselves within the brain and ensure that the nerves and other circuitry function at a better level,” says Jonathan Prousky, ND, MSc. Chronic schizophrenics show higher levels of oxidative stress and cell-membrane breakdown in the frontal cortex and other parts of the brain, as well as lower levels of fatty acids in those areas. That observation, along with evidence that omega-3 supplementation can reduce the incidence and severity of psychosis, leads many clinicians to prescribe fish oil or other sources of omega-3s. (See “How Do Omega-3s Support Mental Health?” for more.)
Niacin
Everyone requires a certain level of niacin, or vitamin B3, in his or her diet, but people with schizophrenia may not only be niacin deficient, they may be niacin dependent, meaning that they require a high dose — up to 3 grams or more daily — to function normally. Andrew Saul, PhD, editor in chief of the peer-reviewed Orthomolecular Medicine News Service, says that Canadian physician and medical researcher Abram Hoffer recommended pairing high doses of B3 with up to 10,000 milligrams of vitamin C, divided into smaller doses throughout the day to increase absorption. “Vitamin C is the body’s most important antioxidant,” Saul says. “Dr. Hoffer believed that, in addition to many other important properties, vitamin C prevented the oxidation of adrenaline to adrenochrome [which Hoffer believed could cause psychotic behavior].”
N-acetylcysteine
Glutathione is a master antioxidant, and it’s produced within the body instead of being absorbed from food. Glutathione helps protect the body from metabolic wear and tear and is especially protective in the brain, a metabolic hot spot where 20 percent of the body’s calories are burned. Research shows that the brains of people with schizophrenia have dangerously low levels of glutathione. One of L.A. psychiatrist Jeffrey Becker’s first steps when treating a schizophrenic patient is to test glutathione levels. If they are low, he starts the patient on a supplement called N-acetylcysteine, or NAC, an antioxidant molecule that provides raw material for the production of glutathione. (For more on the importance of this antioxidant, see ELmag.com/glutathione.)
B6, B12, and folic acid
Many people with schizophrenia have malfunctions in a critical metabolic process called methylation, in which life-giving carbon is passed from vitamins to DNA, fats, proteins, or other molecules. Methylation is essential for health throughout the body and, among other things, affects the building of protein from amino acids and proper gene expression. In the brain, it provides some of the necessary building blocks for neurotransmitters, which are the chemical messengers that ferry signals among neurons as well as other cells in the body. Disruptions to methylation are caused by problems in a gene called methylenetetrahydrofolate reductase (MTHFR), which regulates chemical reactions involving folic acid. When people have two bad copies of this MTHFR gene, they suffer a wide range of problems, including schizophrenia, depression, cancers, spontaneous abortion, and others. Treated with the active form of folic acid — 5-MTHF or 5-methyltetra-hydrofolate — along with B6 and B12 (often injected), many people with schizophrenia feel relief from their symptoms.
Zinc
 Copper from new water pipes, lead from old paint — it’s hard to live in this world without exposure to the heavy metals that can compromise or destroy brain cells. Our bodies are designed to try to get rid of the metals, but people with schizophrenia often have toxic levels of three or more heavy metals. This makes the body’s metal-removing protein, metallothionein, work overtime, which winds up depleting zinc — a good metal that helps us transcribe proteins and create neurotransmitters. “Some people may not be taking in the essential nutrients or protein to make enough neurotransmitters in the brain,” says Becker. “When neurotransmitter levels are low, electricity levels are low in the brain. It’s a dim bulb.” For these reasons, many integrative psychiatrists treat their patients with zinc supplements. (See “Zinc Essentials” to learn more about this building block for healthy cells.)
Copper from new water pipes, lead from old paint — it’s hard to live in this world without exposure to the heavy metals that can compromise or destroy brain cells. Our bodies are designed to try to get rid of the metals, but people with schizophrenia often have toxic levels of three or more heavy metals. This makes the body’s metal-removing protein, metallothionein, work overtime, which winds up depleting zinc — a good metal that helps us transcribe proteins and create neurotransmitters. “Some people may not be taking in the essential nutrients or protein to make enough neurotransmitters in the brain,” says Becker. “When neurotransmitter levels are low, electricity levels are low in the brain. It’s a dim bulb.” For these reasons, many integrative psychiatrists treat their patients with zinc supplements. (See “Zinc Essentials” to learn more about this building block for healthy cells.)
Blood sugar
A diet of 60 to 70 percent healthy fats, 20 to 25 percent protein, and 15 to 20 percent carbs balances blood sugar and helps avoid the kind of blood-sugar spikes that can rattle an already fragile brain.
Food sensitivities
Integrative mental-health practitioners check their schizophrenic patients for food intolerances that might manifest as inflammation in the brain.
Mental Health for Everybody
Just as we should follow a daily regimen that keeps our hearts, skin, and other organs flourishing, we should also be mindful of nourishing our brains, even if we don’t suffer from mental illness. The following tips are designed to keep the jewel in our crowns healthy, and — since everything is connected — may well clear up other problems below the neck.
- Eat more healthy fats: Good sources of omega-3 fatty acids are salmon, herring, sardines, and anchovies, as well as pasture-raised meats and eggs, flaxseeds, walnuts, and omega-3 fish-oil supplements, especially those containing eicosapentaenoic acid (EPA).
- Get more protein: A healthy brain depends on the steady creation of neurotransmitters. The basic building blocks for these transmitters are amino acids that come from the protein in our diets. Experts suggest that 20 to 25 percent of our diets should come from high-quality protein like meat, eggs, dairy, beans, and legumes. And it’s a good idea to begin the day with a solid helping of protein. “I tell people to have dinner for breakfast,” says naturopath Ray Pataracchia. “You might get sick of eggs every day, so you have to change it up and be inventive.”
- Avoid sugar highs: The brain has an enormous need for glucose, and our blood supplies this essential fuel as it circulates through the brain. This supply needs to be slow and steady, without the peaks and valleys caused by simple sugars found in junk food. Stick to the complex carbohydrates found in vegetables, whole grains, and many fruits.
- Buffer stress with B and C vitamins: Stress bombards even the most ordinary lives, both from the outside — a hectic schedule, an angry coworker, commuting to work in heavy traffic — and from the inside, such as when our bodies battle infection and illness. A steady stream of cortisol and other stress hormones can weaken neurotransmitters. Protect them with vitamins C and B — especially niacin, or B3 — which together can regulate and protect these neurotransmitters. The official minimum daily-requirement numbers, says natural-health educator Andrew Saul, PhD, are laughably low: “For someone with a reasonably good diet, a couple hundred milligrams of supplemental B3 would be wise.”
- Stay connected: Robert Hedaya, MD, at the National Center for Whole Psychiatry, compares human beings to neurons: The more connections one neuron has with other neurons, the more vibrant it is. When the connections are severed, a solitary neuron can shrivel and die. Similarly, humans need a connection with other humans and with nature to flourish.
- Develop a spiritual practice: “Fear creates stress,” Hedaya says. “Whatever it is that you’re stressed about, your cognitive framework is going to treat things as more or less stressful. With a spiritual practice, you develop the perspective that there is meaning to life and that we’re not alone. I think the importance of this is highly underrated in the psychiatric field. If you feel as if everything in life is up to you, that’s a lot of pressure. When you add to that the way that so many people live in isolation, that’s a toxic recipe.”



This Post Has 0 Comments