In the fall of 2002, Sarah Ramey was a healthy, active senior in college. On top of a full academic course load, Ramey was directing a musical, singing in an acapella group, and playing in a band. “Except for a persistent urinary tract infection that had started that summer, I was living life and feeling good,” says Ramey.
Ramey never could have anticipated how seeking treatment for such a seemingly minor illness would trigger a prolonged and elusive condition that destroyed her health. Not only were the doctors Ramey saw unable to diagnose or treat her, they implied that her devastating symptoms were psychological, and made her condition worse by suggesting interventions that weren’t appropriate — one of which landed her in the hospital with sepsis.
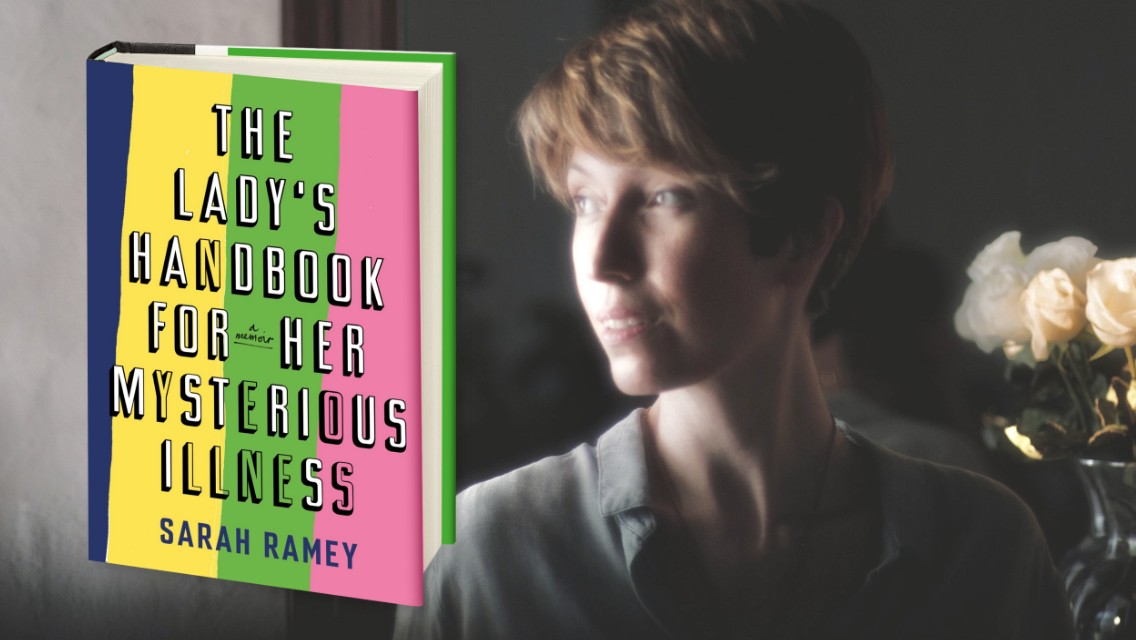
In her darkly funny and courageous medical memoir, The Lady’s Handbook for Her Mysterious Illness, Ramey documents her experience and takes on the taboo subjects of gynecological disorders, chronic illness, and the medical patriarchy, interweaving her own pursuit of a diagnosis and cure with the latest research and a deeply insightful analysis of the state of health care. The result is a page-turning medical mystery that takes you on a roller coaster of emotions from sorrow and anguish to determination and, ultimately, hope.
The Lady’s Handbook for Her Mysterious Illness is a memoir with a mission: to help the millions of women with unnamed or misunderstood conditions — including autoimmune illnesses, fibromyalgia, chronic Lyme disease, and more. Through her own experience with myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), Ramey offers practical advice that others can draw on.
Life Time Editorial | In the process of writing this book you invented a new acronym: WOMI. Tell us about the genesis of the term.
Sarah Ramey | I started writing this book because when I began talking about what was happening to me — about my descent into chronic illness — it turned out that it wasn’t “just me.” It was this enormous group of people, mostly women, with practically identical stories, which is that their health had started deteriorating for unknown reasons and despite seeing countless doctors and submitting to all kinds of tests, they couldn’t get answers about what was going on — or even get a diagnosis.
It was as if in talking openly about my health, I sent up a signal flare, and women started coming out of the woodwork to tell me about their mystery illnesses, which led to the idea of a WOMI — a woman with a mysterious illness — and then to the book.
LTE | One of the themes in your book is medical gaslighting. In your experience, how common is it for female patients to be disbelieved by their doctors?
SR | For the vast majority of women I talk to, that’s their experience of medicine. My parents are both doctors, so I had access to some of the best medical care available. And in the beginning, everyone took what I was experiencing extremely seriously because I’d been so well before and was suddenly so sick.
But as all my tests started coming back negative, a new attitude started to descend on my doctors, which was, “Oh we know what’s going on here! For whatever reason, she believes that she is sick! But she’s not actually sick. She made the whole thing up.”
It was horrifying, obviously, to realize that if you can’t prove you are sick, if you can’t hold up a piece of paper with data, or a picture, or something notarized, then your word is not enough, and you will likely eventually be told some version of “it’s all in your mind.”
LTE | In recent years, the world has started waking up to the injustices women experience at work, at home, and in society. Is medicine another area that needs reform?
SR | When you look at the data, you see that it is extremely common to disbelieve the patient the first five or six times they come to the doctor, especially when it comes to women, people of color, those with a poor socioeconomic status, or LGBTQIA+ patients.
This is a widespread problem in medicine, and we are in this moment of incredible reckoning, where we need to ask the big institutions and people tasked with protecting us, like doctors, to do something that is offensive to their ego. These are people who identify as heroes, but especially in these caring professions, part of the job has to be examining bias and recognizing that some of the ways you treat patients have nothing to do with the data, and everything to do with the way that you, the doctor, feels about the person sitting in front of you.
LTE | When doctor after doctor had no idea how to help you, you finally turned to alternative medicine. What was your experience like in that world?
SR | In the beginning, when I was in that sort of moderately sick stage, it was helpful. I dived into yoga and acupuncture and healthy eating, all of which were new to me. And they did help — in the beginning.
But the longer I was in the alternative-medicine world, the more I realized how much predatory behavior there is that takes advantage of people who are sick by grooming them to believe that happiness, health, and wellness are available to you for the low, low price of a yoga retreat in Bali or a positive-thinking seminar.
There is so much of what I’ve come to call “magical pillthink,” which is the marketing of everything from supplements to kale to yoga as spiritual Paxil. And that’s where alternative medicine can be just as damaging as traditional medicine, where it really does a number on someone’s self-worth. Because the whole premise is that you did this to yourself. That not getting better is a choice.
To be clear, I believe very strongly in the mind-body connection and the power of positive thinking. The mind has an enormous physiologic influence on the body that is well documented. But the mind-body connection is a two-way highway. To think that you can affirm your way to better health is a huge oversimplification of the relationship between the mind and the body.
LTE | When you discovered functional medicine, it came as a tremendous relief. Why does functional medicine give those with chronic illness a reason to be hopeful?
SR | Functional medicine is much more evidenced-based and focused on getting to the root cause of illness by looking at things like nutrient imbalances, hormonal imbalances, gut dysbiosis, the HPA axis, etc. Which means that care plans can be grounded in data.
For the mild-to-moderate WOMI, functional medicine can be really helpful. For the more severely ill WOMI, it’s still going to be a difficult path, no matter what kind of doctor you see — which is why we need to do more research. But even just having somebody who believes you and is trying to help can be very powerful. (For more on the tenets of functional medicine, see “Functional Medicine: A Science Whose Time Has Come”.)
LTE | How did functional medicine change your understanding of chronic illness?
SR | The newest understanding of chronic illness is that it isn’t just the result of bad luck or bad genes. If we use the garden metaphor, for example, your daily behaviors — your food, your microbiome, your sleep, your stress, etc. — all these things make up the soil of your life. If you plant a garden but don’t care for it properly, you can’t grow healthy crops.
So chronic illness, according to functional medicine, is essentially grown out of the soil of your environment, which is a very different way of thinking about the body than traditional medicine. A garden needs to be tended in specific ways, and the human body is exactly the same. It’s another living organism, and certain basic components are needed to maintain robust health.
One of the unavoidable truths of modern life is that we’ve degraded a lot of the basic pillars of health. The quality of the food we eat, the way we take care of our microbiome, how much sleep we get, the amount of stress we have — those things, in the last 60 to 70 years, have really gone out the window.
The wellness movement that’s emerged in the last 20 years is a direct response to the rise of this huge chronic-illness boom. What a lot of the data shows, and functional medicine helps people pinpoint through testing, is that many unexplained illnesses are the result of small, repeated hits to our health that accumulate over time.
What’s so different about chronic illnesses is that they’re not necessarily a top-down illness where there’s one single thing that happened to you, like a virus or a parasite that makes everything fall apart. There is so much evidence to show that a lot of these problems are connected to a disturbance of the microbiome. In some people, that can be the root of the whole illness: Gut dysbiosis leads to a weakened or inflamed immune system, and when a big trauma comes in, such as an infection or injury, it can trigger a neuroinflammatory cascade in an environment that’s essentially a tinderbox.
LTE | Why do we have so little understanding of ME/CFS, fibromyalgia, autoimmune conditions, and other chronic illnesses?
SR | We aren’t investing in research for these conditions — not the way we do with cancer or AIDS, for example. A person with AIDS can have a pretty decent quality of life today, and that’s not magic. It’s because of an enormous amount of funding that came from a massive amount of advocacy.
In the beginning, HIV/AIDS patients were treated atrociously, and in some ways, we see echoes of this with ME/CFS, because many doctors today don’t consider it a real diagnosis and don’t believe the government should spend time or resources studying it. And this situation has been historically true for many illnesses, especially when those illnesses do not prevalently affect straight, white males.
So, while it’s hard to create that unrelenting public pressure, especially when you’re sick, it’s what we need to do to get appropriate medical care. We need to pull together as a community and insist on change.
LTE | Do you have any advice for people dealing with chronic illness about how to advocate for themselves?
SR | I always think the best place to start is with your immediate circle — not with doctors, not with the government, not with social media. For the vast majority of the people I know, so much of the pain of their experience comes from not having the support of the primary people in their life — their partner, parents, friends, or family.
Seeking the support of friends and family can be sticky and difficult for people to take on, but it’s so worth it. Because what ends up happening otherwise is that people might pull away because they may not believe you, they have no idea how to help you, or they may feel intimidated by your illness.
I’ve worked with a lot of people on writing letters to their family or friends to illuminate what it’s like to be inside their body and to live with this illness — in a kind way — and to be really clear about what those individuals can do to help. So, for example, “It would be really helpful to me if we could get a group going that brings me a big batch of soup once a month. And here’s what I can or can’t eat.”
It’s also important to let go of your expectations, because you just don’t know what capacity people have to help. But a lot of people do want to and they just don’t know how. And even if they don’t do something to help you, at least they will start believing you and that alone can be extremely helpful and healing.