Connective tissue is everywhere in the body, so it shouldn’t be surprising that connective-tissue disorders can produce a wide range of health issues. But because conventional medicine tends to divide the body, with specialists focusing solely on individual organ systems, patients sometimes go years without anyone connecting the dots among their symptoms.
“The primary systems where we tend to see consistent problems in this population are the nervous, immune, and gastrointestinal systems,” says Patty Stott, DPT, ATC, CHT, who works with hypermobile patients in Arvada, Colo. “These systems tend to be less efficient on a cellular level. But that gives us a lot of access points to figure out where an individual needs support.”
In addition to joint hypermobility, these are some of the most common conditions seen in people with hEDS or HSD.
1) Postural orthostatic tachycardia syndrome (POTS)
This syndrome involves rapid heart rate, fatigue, and dizziness when standing up. “POTS is seen with more frequency in our patient population than in the general population, though still not the majority,” says Dacre Knight, MD, medical director of the Ehlers-Danlos Syndrome Clinic at Mayo Clinic in Jacksonville, Fla.
Symptoms are caused by dysregulation of the autonomic nervous system (ANS), which governs processes such as heart rate, breathing, and digestive function.
POTS is also associated with an overactive sympathetic nervous system, which governs our fight-or-flight response. This can interfere with sleep, digestion, energy, and cognition. One theory about the connection between hEDS and POTS is that lax connective tissue in the blood vessels may lead to faulty blood-pressure control.
2) Mast cell activation syndrome (MCAS)
Mast cells are the body’s first responders to foreign invaders. They deploy a large arsenal of chemical mediators to head off various dangers, including enzymes that damage connective tissue.
Researchers have noted a subset of long-COVID patients who develop pain and joint hypermobility; mast cells are a potentially critical link. “It may be that viruses activate mast cells, causing damage from inflammation, which translates to weakening joints, tendons, and ligaments,” Knight explains, adding that the research into a potential long COVID–hEDS link is still in its early stages.
3) Fatigue and brain fog
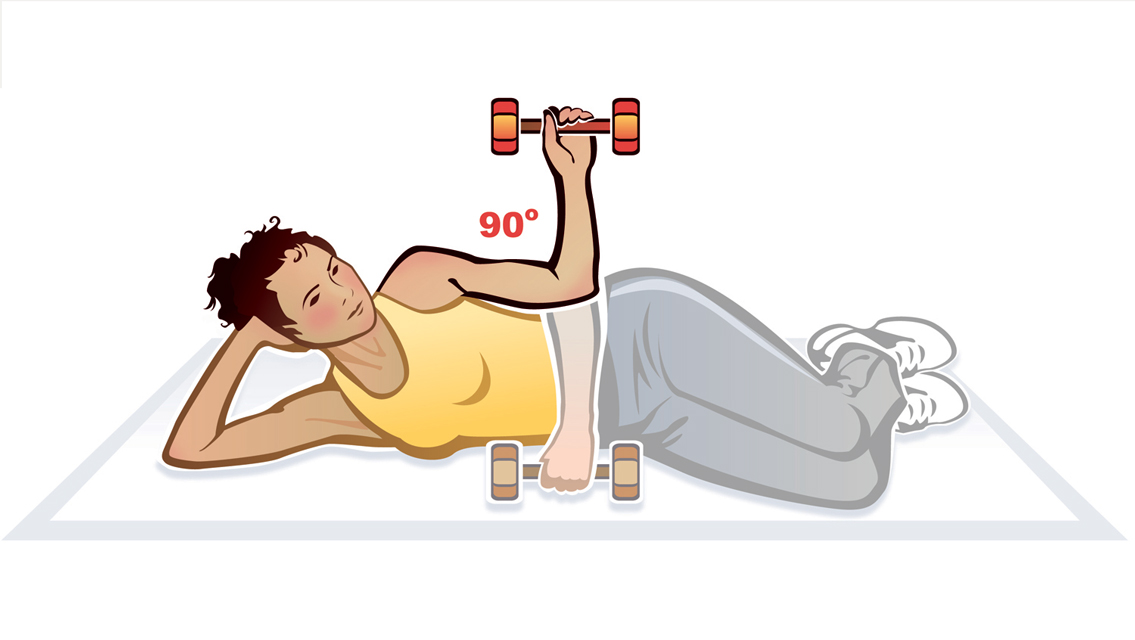
More than three-quarters of Knight’s hEDS and HSD patients report fatigue and brain fog. He suggests a couple of possible causes. “One, the muscles are having to work harder to stabilize the joints. Another reason for fatigue is that a lot of patients have injuries and chronic pain, which can lead to deconditioning.”
When exercise tolerance flags, even low levels of exertion can feel exhausting. “It’s important that we encourage patients to find some form of healthy, safe, physical activity they can do to prevent this,” Knight says. “If it’s not prevented, it can lead to a vicious cycle of fatigue where little activities like walking up the stairs become really fatiguing.”
Finally, unrefreshing sleep (which can go hand in hand with pain or a dysregulated ANS) can contribute to feeling chronically fatigued.
4) Anxiety
An Iranian study, published in 2020, found that hypermobility was three times more prevalent in children with anxiety disorders than in those without. And a 2014 study in Frontiers in Psychology found that people with hypermobile joints have heightened brain activity in brain regions associated with anxiety.
Stott notes that electrical and functional problems in the ANS of people with hEDS or HSD may help explain this; it’s like faulty wiring. “The ANS digests all our life experiences just like the GI system does with food. When hypermobility is present, we see inefficiency in this system. When it isn’t working optimally, you’re going to get faulty messages.”
A dysregulated ANS and anxiety can get into a feedback loop, with anxiety exacerbating dysautonomic symptoms of rapid heart rate, shallow breathing, and dizziness, and vice versa. Those with a history of trauma, adverse childhood experiences, or chronic stress may be particularly challenged.
5) Digestive issues
Gut-health issues are another common problem for people with connective-tissue disorders. The intestines are made of connective tissue, and laxity there can impede the movement of food and stool through the digestive tract.
The parasympathetic nervous system, which puts us into rest-and-digest mode, may also be underactive in people with hEDS or HSD, leading to functional gut issues. “IBS, nausea, and bloating are quite significant and very common in people with hEDS or HSD,” says Knight.
This was excerpted from “What Is Connective-Tissue Disorder?” which was published in Experience Life.



This Post Has 0 Comments