I’ve been spending an inordinate amount of time in the company of healthcare professionals lately, thanks to a “hypertensive crisis” that drew rapt attention to a spike in my chronically high blood pressure. Those numbers have stabilized since I began taking a couple of medications each morning, and I’ve humbly accepted the previously unacceptable fact that the genetic lottery — and my advanced age — make pharmaceutical remedies necessary in this case. But I’m less sure about statins.
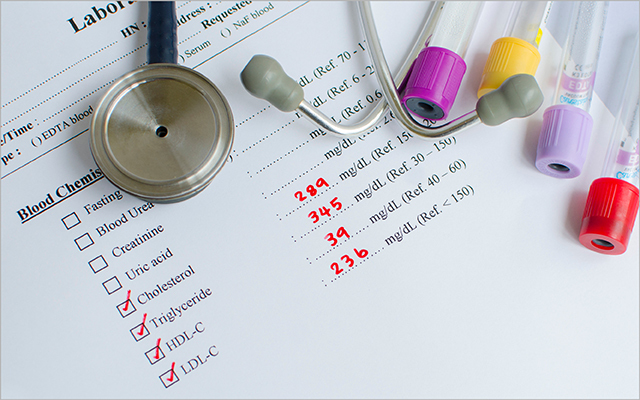
The results of recent blood tests revealed that I’m harboring a robust collection of “bad” LDL cholesterol, which generally signals the accumulation of arterial plaque and increases the threat of a stroke, heart attack, and other unpleasant occurrences. Statins of various brands have long been prescribed to reduce the risk of such calamities, but along the way they’ve acquired a reputation for producing a range of side effects — type 2 diabetes, liver dysfunction, muscle and joint pain — that are similarly unsettling.
So, I arrived at my local clinic last Friday armed with a few highlights from recent research and a vague hope that my doctor and I might reach some consensus about the threat that my high cholesterol count presents and the risks and benefits of a potential statin regimen. It’s a tall order, considering how much disagreement exists among researchers — especially when dealing with seniors.
A 2022 study from RCSI University of Medicine and Health Sciences in Ireland, for instance, found the link between high cholesterol and heart disease to be “inconsistent.” And, the pharmaceutical watchdog Choosing Wisely argued in a 2017 report that the association is particularly tenuous among the elderly. “There is no evidence that hypercholesterolemia, or low high-density lipoprotein cholesterol is an important risk factor for all-cause mortality, coronary heart disease mortality, or hospitalization for myocardial infarction or unstable angina in persons older than 70 years,” officials there noted. “In fact, studies show that elderly patients with the lowest cholesterol have the highest mortality after adjusting other risk factors.”
Meanwhile, a study published in the Annals of Internal Medicine questions the guidelines physicians use when prescribing statins, arguing that older patients must present a very high risk of heart disease to reap a net benefit from the drugs. Plus, the authors added, “the level of risk at which net benefit occurs varies considerably by age, sex, and statin type.”
My pharmaceutical-averse self tends to cling to such evidence until faced with credible data that counters my jaundiced worldview. And, as Jane Brody notes in the New York Times, there hasn’t been much credible data to persuade septuagenarians like me to take the statin plunge. “As is true in most drug trials on new medications,” she writes, “relatively few people over 75 were included in early studies that assessed the benefits and risks of statins.”
Three recent studies, however, claim to offer some reassurance for elderly statin users:
- A French study involving more than 120,000 seniors found that those who stopped using the drug were 25 to 30 percent more likely than their counterparts who kept taking the pills to land in the hospital with cardiovascular trouble.
- Israeli researchers, meanwhile, tracked 20,000 elderly statin users for 10 years and concluded that they were 34 percent less likely than those who discontinued the protocol to die from any cause.
- And a survey of 326,981 elderly U.S. veterans found that statin use was associated with 25 percent fewer deaths than nonuse during a seven-year period.
Each of these studies, however, included enough caveats to invite skepticism, which I shared with my physician, who agreed that we should proceed with caution. Still, those cholesterol numbers don’t lie, she noted, and I admitted that they’d probably been elevated for years.
“And yet,” I smugly pointed out, “I’m still here: no stroke, no cardiac arrest.”
“We don’t know that for sure,” she replied. “You may have had a heart attack without knowing it.”
She could order an echocardiogram to determine whether any of my heart tissue shows the type of damage that would indicate I’d suffered such an attack in the past — something I’d never considered — but first she wanted to find out whether there was any blockage in my arteries. Only then could she recommend a statin regimen.
As she described the coronary calcium scan, I found myself mildly distracted by the possibility that I may have already survived what’s known as a “silent” heart attack. I couldn’t recall any incident that might have signaled such a breakdown of my cardiovascular system, but that doesn’t mean it couldn’t have occurred. It often appears as simple heartburn, flu-like symptoms, or a strained chest muscle. Been there, I mused. Felt that.
So, it appears I’m going to become even more familiar with our sprawling healthcare system in the weeks ahead, a prospect that would have sparked a panic attack even a month ago but feels now like the new normal. As I thanked my doctor for her patience and cautious advice, she motioned toward the exit.
“Oh, I know my way out,” I assured her. “This is like my home away from home now.”




This Post Has 0 Comments